Introduction And Basics
Gynecomastia, also known colloquially as ‘gyno’ and more informally as ‘bitch tits’, is the abnormal and unusual development of breast tissue on the chest region. Gynecomastia in particular almost always refers to the development of breast tissue on males rather than females, whom the development of breast tissue is a normal expected occurrence. It is a recognized medical disorder that can develop as the result of many different causes, but specifically it is caused by the actions of Estrogen, Estrogen analogues, or estrogenic compounds and/or substances (such as phytoestrogens from plastics, plants, foods, etc.) on the receptor sites of breast tissue in the chest and nipple area. This normally occurs in a hormonal environment that is unbalanced in favor of high or excessive Estrogen levels. Gyno will typically manifest itself as the growth of additional glandular tissue, and in the case of anabolic steroid use, will typically be the result of heightened Estrogenic activity resulting from high amounts of aromatization (the conversion of androgens into Estrogen) or the result of anabolic steroids that exhibit estrogenic activity in and of themselves (such as Anadrol-50, for example).
Although Gynecomastia tends to occur as the result of excessive Estrogen levels in the body, it can also occur in the presence of normal Estrogen levels as well, though this is a far rarer occurrence that will be described and explained in greater detail very shortly. For the time being, it should be understood that Gynecomastia is typically the result of excessive Estrogen levels. Various causes of such occurrences include puberty, genetics, individual sensitivity, and the activity of other hormones in the body such as Progesterone. All of these will be expanded upon later on in this article, as the main concern here is Gynecomastia resultant of anabolic steroid use. It is also very important to note that not all anabolic steroids hold the capability to aromatize into Estrogen, and therefore cannot possibly exhibit or aggravate gyno, and in fact the majority of anabolic steroids are void of the ability to produce gyno. It so happens, however, that some of the most effective and popular anabolic steroid analogues tend to also be those which aromatize at a moderate to high amount into Estrogen. Some examples are Dianabol (Methandrostenolone), Testosterone, or Equipoise (Boldenone), each of which will aromatize into Estrogen to varying degrees and rates when utilized at bodybuilding or performance enhancing doses.
One particular point that should be made very clear about gyno, however, is the fact that while Gynecomastia might be regarded as a frequent or common side effect of anabolic steroid use, it is in fact the most easily avoidable side effect.
The general description of how Gynecomastia is formed at the cellular level is as follows: Estrogen is the prime culprit in the development and support of gyno, where it binds with Estrogen receptors located within breast tissue, and through receptor signaling, will catalyze and contribute to the growth of ductal tissue (specifically referred to as ductal epithelial hyperplasia) as well as ductal elongation and branching, and fibroblast proliferation[i]. In other words, Estrogen will (through interaction with Estrogen receptors on breast tissue) signal the growth and development of the mammary gland, milk ducts, and breast tissue. While estrogens act to promote growth of breast tissue, it is very important to note that androgens serve to inhibit breast tissue growth[ii]. This makes logical sense, considering the fact that Dihydrotestosterone (DHT) is one of the body’s natural and quite effective anti-estrogens. In summary of this explanation, these details tell us that Gynecomastia can only formulate in the appropriate hormonal environment necessary for the favor of the development gyno.
The development of Gyno is certainly not restricted to anabolic steroid using bodybuilders or athletes, and as previously mentioned, it can occur as the result of puberty. Pubertal development of gyno is known as perhaps the second most popular cause of the disorder among males, but is actually experienced in greater numbers by males than anabolic steroid induced Gynecomastia. Pubertal Gynecomastia (or puberty induced Gynecomastia) is the result of fluctuating hormone levels as a result of the normal hormonal developments during puberty, which in many young males can generate high or excessive Estrogen levels that can indeed rise high enough to initiate and facilitate the development of gyno. Puberty related gyno is fairly common, with estimates at roughly 50% or more of all adolescent males having developed Gynecomastia[iii] [iv]. It has been found, however, that 75% of all pubertal Gynecomastia cases will self-resolve without any medical intervention or treatment within two years of onset[v]. Older men around and above 45 years of age who experience the natural decline of Testosterone levels (the condition known as Andropause) are also known to develop Gynecomastia, as the hormonal environment in older men tend to shift in favor of excessive Estrogen levels and low androgen levels[vi]. Obesity and excessively high body fat percentages in men also contributes to the disorder of Gynecomastia as clinical studies have demonstrated that a higher body fat percentage will present a higher risk of Estrogenic side effects[vii]. This is because the aromatase enzyme is highly abundant in adipose tissue, and so it stands to reason that the higher an individual’s body fat percentage is, the greater the rate of aromatization of androgens into Estrogen will result.

Gynecomastia before and after surgery
Gynecomastia is an often mocked side effect of anabolic steroid use among the general uneducated public, though the majority of people and individuals know relatively nothing about the complexity and varying factors concerning it. It is, for the most part, a cosmetic side effect that is considered unattractive and unappealing, but not life-threatening. The unsightly nature of this side effect is what has prompted the mocking of its association with anabolic steroids, and the degree to which the development of gyno on an individual manifests and presents itself will vary greatly, ranging from minor and almost unnoticeable to larger, more noticeable, and can be very feminine in its display, all being very difficult to conceal. Gyno, for the most part, is generally the result of either ignorance, neglect, or impatience on the part of the anabolic steroid user himself. The majority of Gynecomastia cases that result from anabolic steroid use are usually the result of an individual who is uneducated on the general use of anabolic steroids and the proper prevention/care of the various side effects. In this day and age with the ease of access to mounds of medical and scientific information as well as the proper compounds, supplements, and drugs to assist in the prevention/resolution of an issue such as Gynecomastia, there is really no excuse for any anabolic steroid user to succumb to the full development of gyno. Unlike 40 years ago, ignorance of the proper and responsible use of anabolic steroids is no excuse.
For those who wish to learn about the complexity of the development of gyno at the cellular level as well as the proper preventative measures (and even the purported measures for reversal), this article will efficiently and thoroughly describe and educate the reader concerning these topics. Following the reading of this article, the reader can expect to be thoroughly educated and prepared for the prevention and/or treatment of the potential of breast growth.
Anabolic Steroid Induced Gynecomastia
As previously mentioned, we are concerned almost exclusively with anabolic steroid induced Gynecomastia rather than any other particular forms. But whatever the origin or cause of gyno might be, the end result of Gynecomastia formation is the same, and normally ultimately caused by the same hormonal functions/disruptions at the cellular level. In the case of anabolic steroid induced gyno, the initial cause must first be identified and explained. It has been previously mentioned thus far that the vast majority of anabolic steroid analogues actually do not possess the ability to cause Gynecomastia, but only a handful do. There are various other compounds that can directly contribute to and aggravate Gyno directly (where the hormone is hypothesized to interact directly with the Estrogen receptors in breast tissue), while most compounds will exacerbate Gynecomastia via aromatization into Estrogen, and there are also compounds that can contribute to Gynecomastia indirectly (through other pathways that do not involve aromatization).
It is important to understand which anabolic steroids are of concern when it comes to the issue of gyno and what relation these compounds have with the development of Gynecomastia. Reiterating from earlier in this article, it happens to be that some of the most effective and popular anabolic steroids tend to also be those which aromatize at some varying rate and degree into Estrogen. The following is a breakdown of the various compounds of concern when it comes to Gynecomastia.
Aromatizable Anabolic Steroids (High rate of aromatization):
– Cheque Drops (Mibolerone)
– Methyltestosterone
Aromatizable Anabolic Steroids (Moderate rate of aromatization):
– Testosterone (all esters and blends)
– Dianabol (Methandrostenolone)
Aromatizable Anabolic Steroids (Low rate of aromatization):
– Deca-Durabolin (Nandrolone Decanoate)
– Equipoise (Boldenone Undecylenate)
– Nandrolone Phenylpropionate
Directly Estrogenic Anabolic Steroids:
– Anadrol 50 (Oxymetholone)
Progestational Anabolic Steroids:
– Deca-Durabolin (Nandrolone Decanoate)
– Nandrolone Phenylpropionate
– Trenbolone
It stands to reason that the higher the rate of aromatization, the more likely a hormonal environment favoring an excess of Estrogen will develop, which will then increase the likelihood of the development of Gynecomastia. This occurs by way of their affinity for the aromatase enzyme (the enzyme responsible for the aromatization of the androgen into Estrogen), and some androgens exhibit low, moderate, or high affinity for interaction with the aromatase enzyme. Anabolic steroids that are directly estrogenic, such as Anadrol 50 (Oxymetholone), are anabolic steroids that do not aromatize into Estrogen at any dose but will still exhibit estrogenic activity in and of themselves (or as a result of their metabolites) upon the Estrogen receptor in breast tissue. Progestational anabolic steroids, also known as Progestins, might not convert into Estrogen at all (such as Trenbolone) but can possibly cause or aggravate Gynecomastia even further by way of Progestin interaction with the Estrogen receptor, which can cause or create Gynecomastia even though normal physiological Estrogen levels are present. All other anabolic steroids that are not listed above (such as Anavar (Oxandrolone), Winstrol (Stanzolol), Primobolan (Methenolone), or Masteron (Drostanolone)), being that they are Dihydrotestosterone derivatives, do not and cannot aromatize into Estrogen at any dose at all and therefore present no risk of producing or aggravating Gynecomastia on their own.

Gynecoastia from anabolic steroid abuse
The issue of Progesterone and Progestogenic anabolic steroids and their effects on Gynecomastia is a highly misunderstood one among the bodybuilding and anabolic steroid using community. It is important to clarify this misunderstanding and shed light on the proper understanding of this hormonal component, as often times individuals might utilize an anabolic steroid that does not exhibit any Estrogenic effects at all (such as Trenbolone), and yet they will experience development of Gynecomastia, and become baffled as to why. Although Estrogen is the primary culprit and the key component in Gyno, Progesterone and Progestogenic anabolic steroids and hormones, have been known to also play a key role in the development of Gynecomastia in the sense that they potentiate the effects of Estrogen on breast tissue growth[viii]. Both Estrogen receptors as well as Progesterone receptors exist within breast tissue, and it is understood that the activity at the Estrogen receptor will increase/amplify the sensitivity/reactivity of the Progesterone receptor. The vice-versa effect can occur as well, where Progestins can and do increase the affinity/sensitivity of the Estrogen receptor for Estrogens.
In other words, anabolic steroids that possess a high degree of Progestational (AKA Progestogenic) activity, such as Nandrolone (Deca-Durabolin) or Trenbolone, through interaction with the Progestersone receptor can potentially ‘excite’ the Estrogen receptor and increase the Estrogen receptor’s affinity and receptivity to any Estrogens circulating within the bloodstream. The result is an increased sensitivity to Estrogenic effects in breast tissue, which will invariably result in Gynecomastia (or the increased probability of developing it). Because of the increased sensitivity of the Estrogen receptor created by Progestational activity, Gynecomastia formulation can occur even with normal physiological blood plasma levels of Estrogen. This intricate matrix of Estrogen, Estrogen receptors, Progesterone, and Progesterone receptors creates a network by which Gynecomastia can become a significant issue that is not only attributed to excessive Estrogen levels. The use of a SERM (Selective Estrogen Receptor Modulator) or an AI (Aromatase Inhibitor) in these situations is normally adequate to mitigate Gynecomastia that is caused by Progestogenic anabolic steroids through their combative effects on the Estrogen component of this issue, but the proper and efficient use of AIs and SERMs in order to treat or prevent gyno will be explained in further detail very shortly.
The one final related component/issue that is related to Gyno is the hormone known as Prolactin, which is a hormone that can be increased through the use of various anabolic steroids, but is known to become increased through the use of 19-nor Progestins such as Trenbolone and/or Nandrolone (Deca-Durabolin). Although Prolactin will not contribute to breast tissue formation and has nothing to do with Gynecomastia in and of the disorder, it is a hormone that can and will cause lactation of the nipples if blood plasma levels rise to excessive levels. The nipple area can commonly take on a puffy look and exhibit clear fluid secretion in men (lactation). Sometimes this can occur alongside actual Gynecomastia and often be mistaken for “Prolactin-induced Gynecomastia” which is actually a misnomer, and is normally associated with Gynecomastia due to the relation of effects in the nipple area. Excessive Prolactin levels can be effectively reduced through the utilization of a Prolactin antagonist (also known as a dopamine agonist) such as Cabergoline, Bromocriptine, or Pramipexole. Vitamin B6 has also demonstrated significant capability in reducing Prolactin levels in the body[ix] [x] [xi].
Overall, Gynecomastia and the mechanisms behind its development at the hormonal and cellular level is indeed extremely complex, being that there are so many different pathways to its development. The causative factors are very complex, and its specifics are largely unknown to the medical establishment. There are a number of contributing agents that include Estrogens, Progestins, Growth Hormone, IGF-1, and Prolactin that might be involved. The bottom line, is, however, that most medical experts in this particular disorder believe that a decreased androgen:Estrogen ratio (in favor of high Estrogen) is the definitive component for the development of gyno, and that blocking Estrogen’s activity, reducing total serum levels of Estrogen, or increasing Testosterone and DHT levels, is the prime core component to addressing the issue of Gynecomastia. Prolactin is not a core contributing issue, but it is one of the contributing factors. The same can be said for Progesterone and Progestins, as influential as they might be. Gynecomastia is a complex disorder that is comprised of many gears that run the machine, whereby if one or more of the gears can be effectively removed or stopped, the whole machine of Gynecomastia can be effectively stopped.
Diagnosis, Prevention, and Treatment of Gynecomastia
Following an understanding of how Gynecomastia works and develops at the cellular level (including its hormonal causes and interactions), it will be much easier to understand the methods of treatment and prevention of the disorder (including the drugs and compounds to be utilized for such purposes). Initially, however, an actual case of Gyno must be first properly diagnosed. All too often, many individuals tend to think they are exhibiting symptoms of Gynecomastia when they really are not, and their misconception of gyno is a result of over-concern, fear, and a lack of comprehension of the proper symptoms of the condition. One particular point is very clear about gyno, however, and that is the fact that while Gynecomastia might be regarded as a frequent or common side effect of anabolic steroid use, it is in fact the most easily avoidable.
Diagnosis
Diagnosis of gyno is fairly simple and straightforward, as there are some prominent and distinct signs and symptoms of Gynecomastia that are unmistakable even to the untrained eye or someone who is not a medical professional. There is rarely any guessing or uncertainty involved in the identification and diagnosis. The speed or rate at which the development of gyno occurs can vary through its different developmental stages. This also includes the intensity and severity of growth, all of which depend on many factors, such as: the type of anabolic steroid(s) used, doses, duration of use, as well as perhaps the single most important factor, which is the individual’s sensitivity to Gynecomastia. Some might never experience gyno despite increases of Estrogen to massive excess, while other individuals can experience sudden onset of Gynecomasta in the midst of the ever so slightest rise in the levels of circulating Estrogen.
Development of Gynecomastia can occur both bilaterally or unilaterally[xii] [xiii]. This is to say that it is not a requirement for gyno to occur on both sides of the chest at the same time, and can (and frequently does) occur on one side of the chest only. Gyno can also present itself as slight development on one side of the chest while there is significant development on the other side of the chest. Significantly increased diameter of the areola (the circular area around the nipple) and/or significant asymmetrical chest tissue development reminiscent of the previous descriptions are also signs of gyno[xiv]. Upon consultation with medical professionals, ultrasonography is typically utilized for radiologic assessment of the breast tissue for the diagnosis of Gynecomastia[xv]. Examination of breast tissue extracted by fine-needle aspiration can also be conducted in order to examine the tissue for dilated ducts that exhibit periductal fibrosis, subareolar fat tissue increases, as well as stroma hyalinization[xvi].
Gynecomastia is also categorized into different stages of development:
1. Sensitivity and pain in and/or slightly beneath the nipple area (medically referred to as gynecodeynea).
2. Significant swelling (also described as ‘puffiness’) of the nipple area (medically referred to as lipomastia). At such point, glandular tissue has not developed yet, and this is generally considered the reversible point of Gynecomastia development.
3. Complete Gyno development (complete glandular growth and development as well as complete fatty tissue development has been achieved at this point, at which Gynecomastia is irreversible without surgery).
The speed at which these stages progress to one another depends on many variables (such as the hormonal environment, aggravating agents, and other causative factors). The aforementioned stages can progress as rapidly as two to three days, or it can progress as slowly as a number of weeks. Some cases of Gynecomastia can linger at any of the three stages for weeks or even months before progressing to the next development stage (or regressing).
The degree of severity of breast growth has even been categorized into a grade system by the medical establishment[xvii]:
Grade 1: Minor enlargement with no skin excess.
Grade 2: Moderate enlargement with no skin excess.
Grade 3: Moderate enlargement with skin excess.
Grade 4: Marked enlargement with skin excess.
Prevention and Treatment
The methods of both prevention and treatment of Gynecomastia are very closely related, especially in terms of the medications and compounds utilized in order to mitigate or avoid Gynecomastia. Prevention will require techniques other than the use of any additional compounds, substances, or supplements, which will be described in detail shortly. However, the different tools at one’s disposal for either the prevention or treatment of Gynecomastia should be fully understood and these must first be covered and described in detail. Following this, the typical proper use of these compounds will be briefly described.

Gynecomastia is a build up of breast tissue
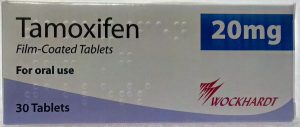
Selective Estrogen Receptor Modulators (SERMs) – SERMs are perhaps the most typical example representative of the first line of attack (as well as defense) against Gynecomastia. SERMs were in fact developed for complications related to breast tissue growth, namely Estrogen responsive breast cancer. Because Estrogen responsive breast cancers operate via the same hormonal pathways that Gynecomastia does, the use of SERMs to prevent, inhibit, or halt the development of gyno have proven to be extremely effective[xviii]. However, the official use of SERMs as a treatment for Gyno has not been approved by the FDA[xix]. At the cellular level, SERMs act to specifically block the activity of Estrogen in breast tissue by way of occupying the Estrogen receptor sites so that Estrogen itself cannot bind to these receptors. This is otherwise known as Estrogen antagonism. Although SERMs exhibit effects elsewhere in the body, the concern in this case in particular is with the prevention and/or treatment of gyno. It is important to note that SERMs do not lower total circulating Estrogen levels in the body – they simply serve to block Estrogen’s effects in and upon various tissues. Various SERMs include: Nolvadex (Tamoxifen), Clomid (Clomiphene), Fareston (Toremifene), Evista (Raloxifene) and others.
Tamoxifen Citrate gynecomastia treatment and prevention
Aromatase Inhibitors (AIs) – Unlike SERMs, AIs will serve to actually lower total circulating plasma levels of Estrogen in the body, thereby reducing Estrogen levels to normal physiological levels (or much lower) if Estrogen levels have risen to very high levels that are typically responsible for the development of Gynecomasta. Estrogen is generated by way of the conversion of aromatizable androgens (such as Testosterone) into Estrogen, which is a process known as aromatization. The enzyme responsible for this aromatization is known as aromatase. AIs will act to effectively inhibit the activity of aromatase by binding to it, disallowing it to exert its effects on circulating Testosterone (or any other aromatizable androgens). The disabling of the aromatase enzyme results in an inability for Estrogen to be produced, thereby resulting in a reduction of total Estrogen levels in the body. Some AIs, such as Arimidex and Letrozole, will only temporarily inhibit the enzyme while other AIs (such as Aromasin) will permanently disable the enzyme. AIs that permanently disable the aromatase enzyme are known as suicidal inhibitors, and although the existing enzymes at the time of administration might become permanently inhibited, the body will eventually manufacture more aromatase to restore its normal physiological amounts. Aromatase inhibitors vary in strength and potency in how efficiently they will inhibit aromatase, ranging from from very mild (such as Proviron) to very strong (such as Letrozole). Various AIs include: Aromasin (Exemestane), Arimidex (Anastrozole), Femara (Letrozole), Proviron (Mesterolone), and others.
Dihydrotestosterone (DHT) creams – There is some anecdotal evidence that Dihydrotestosterone creams have the potential to prevent or reverse gyno by way of topical application right on the nipple and chest area (direct rubbing of the cream into the area). Although there is no clinical data to support these claims, there are individuals both within the bodybuilding / anabolic steroid using community as well as outside of it that have claimed success in stopping or preventing Gynecomastia development through the use of a DHT cream as a last resort, normally after all other medications and treatments have been attempted. It is understood that Dihydrotestosterone and Testosterone (androgens in general) play a crucial role as naturally occurring endogenous anti-Estrogens in the body[xx], and that through this understanding, there indeed might be an application in the use of topical DHT creams in combating Gynecomastia.
It should be carefully noted and remembered by any and all readers that although these medications and substances can effectively stop the development of Gynecomastia in its tracks (or possibly reverse Gynecomastia shortly after its development has begun), the medical establishment has determined that breast growth that has been established for over one full year (or that has grown beyond an irreversible stage), surgical removal is normally required for complete removal[xxi].
Specific Use of the Aforementioned Compounds For the Prevention of Gynecomastia
The cheapest, most commonly used, and most effective SERM to date is Nolvadex (Tamoxifen) for the prevention and treatment of Gynecomastia, and therefore Nolvadex will be utilized as the sample compound for the purpose of description here. Arimidex (Anastrozole) and Aromasin (Exemestane) tend to both be almost equal in popularity of use for the treatment and prevention of Gynecomastia as far as aromatase inhibitors are concerned, and so they will be utilized as further examples as well. It is initially up to the user as to which method of gyno prevention to adopt during an anabolic steroid cycle. There are generally three effective methods of prevention:
1. Dose adjustment and/or moderate dose – The most cost-effective method of Gynecomastia prevention that will not result in the possible interference with gains or health is that of simple dose adjustment and/or the selection of anabolic steroid(s). Generally speaking, it can be said that the less compounds one should require, the better. The decision to select a sensible dose or anabolic steroid would eliminate the necessity to add a daily administration of a SERM or an AI into a cycle. For example, running a cycle that involves TRT doses of Testosterone (no more than 100mg per week) while emphasizing the use of a non-aromatizable anabolic steroid such as Winstrol or Anavar through a slightly increased dose will ensure that the user maintains a low enough dose of Testosterone so that little to no aromatization will occur.
2. SERM use during cycles – Simply put, this involves the use of a SERM, such as Nolvadex, on a daily basis throughout an anabolic steroid cycle, typically at a dose of 20mg per day. This would effectively block the Estrogen receptor located within breast tissue so that any excess Estrogen cannot bind to it and stimulate the development of gyno. Chronic use of a SERM such as Nolvadex, however, has been shown to reduce levels of IGF-1 in the body significantly by approximately 30%[xxii], which might possibly impact potential gains in a significant manner.
3. AI use during cycles – The daily (or every other day) use of an AI such as Arimidex or Aromasin during an anabolic steroid cycle at 0.5mg and 12.5mg respectively is generally a common practice among the bodybuilding and anabolic steroid using community. The key in this case is the control of Estrogen levels,
Medical References:
[i] Estrogen regulation of mammary gland development and breast cancer: amphiregulin takes center stage. Heather L LaMarca and Jeffrey M Rosen. Breast Cancer Res. 2007; 9(4):304.
[ii] Androgens and mammary growth and neoplasia. Dimitrakakis C, Zhou J, Bondy CA. Fertil Steril. 2002 Apr;77 Suppl 4:526-33.
[iii] Gynaecomastia and breast cancer in men. Niewoehner, CB; Schorer, AE (March 2008). BMJ 336 (7646): 709–713. doi:10.1136/bmj.39511.493391.BE. PMID 18369226.
[iv] Disorders of the Testes and Male Reproductive System Harrison’s principles of internal medicine (17th ed. ed.). Chapter 340. Fauci, Anthony S.; Eugene Braunwald, Dennis L. Kasper , Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Kurt J. Isselbacher (2008). New York: McGraw-Hill. ISBN 978-0-07-147693-5.
[v] Use of aromatase inhibitors in children and adolescents with disorders of growth and adolescent development. Shulman, DI; Francis, GL; Palmert, MR; Eugster, EA; Lawson Wilkins Pediatric Endocrine Society Drug and Therapeutics Committee (April 2008). Pediatrics 121 (4): e975–983. doi:10.1542/peds.2007-2081. PMID 18381525.
[vi] Gynecomastia: pathophysiology, evaluation, and management. Johnson, RE; Murad, MH (November 2009). Mayo Clinic Proceedings 84 (11): 1010–1015. doi:10.1016/S0025-6196(11)60671-X. PMID 19880691.
[vii] Aromatization of androstenedione and 19-nortestosterone in human placental, liver, and adipose tissues (abstract). Nippon Naibunpi Gakkai Zasshi 62 (1986:18-25
[viii] Roles of estrogen and progesterone in normal mammary gland development insights from progesterone receptor null mutant mice and in situlocalization of receptor. Shyamala G. Trends Endocrinol Metab. 1997 Jan-Feb;8(1):34-9.
[ix] Effect of pyridoxine on human hypophyseal trophic hormone release: a possible stimulation of hypothalamic dopaminergic pathway. Delitala G, Masala A, Alagna S, Devilla L. J Clin Endocrinol Metab. 1976 Mar;42(3):603-6.
[x] Pyridoxine (B6) suppresses the rise in prolactin and increases the rise in growth hormone induced by exercise. Moretti C, Fabbri A, Gnessi L, Bonifacio V, Fraioli F, Isidori A. N Engl J Med. 1982 Aug 12;307(7):444-5.
[xi] [Influence of administration of pyridoxine on circadian rhythm of plasma ACTH, cortisol prolactin and somatotropin in normal subjects]. Boll Soc Ital Biol Sper. 1984 Feb 28;60(2):273-8. Barletta C, Sellini M, Bartoli A, Bigi C, Buzzetti R, Giovannini C.
[xii] Current concepts in gynaecomastia. Devalia, HL; Layer, GT (April 2009). Surgeon 7 (2): 114–119.
[xiii] Gynecomastia. Dickson, G (April 2012). American Family Physician 85 (7): 716–722.
[xiv] Algorithm for clinical evaluation and surgical treatment of gynaecomastia. Cordova, A; Moschella, F (2008). Journal of plastic, reconstructive, & aesthetic surgery 61 (1): 41–49.
[xv] Gynaecomastia: an endocrine manifestation of testicular cancer. Hassan, HC; Cullen, IM; Casey, RG; Rogers, E (June 2008). Andrologia 40 (3): 152–157. doi:10.1111/j.1439-0272.2007.00815.x. PMID 18477201.
[xvi] Algorithm for clinical evaluation and surgical treatment of gynaecomastia. Cordova, A; Moschella, F (2008). Journal of plastic, reconstructive, & aesthetic surgery 61 (1): 41–49.
[xvii] Minimally invasive esthetic procedures of the male breast. Wollina, U; Goldman, A (June 2011). Journal of cosmetic dermatology 10 (2): 150–155. doi:10.1111/j.1473-2165.2011.00548.x.
[xviii] Treatment of marked gynecomastia in puberty with tamoxifen. König R, Schönberger W, Neumann P, Benes P, Grimm W. Klin Padiatr. 1987 Nov-Dec;199(6):389-91.
[xix] Drug-induced gynecomastia: an evidence-based review. Deepinder, F; Braunstein, GD (2012). Expert opinion on drug safety 11 (5): 779–795. doi:10.1517/14740338.2012.712109. PMID 22862307.
[xx] Role of testosterone and dihydrotestosterone in spontaneous gynecomastia of adolescents. Villalpando S, Mondragón L, Barrón C, Pérez-Pastén E, Castañeda G, Alonso-Uriarte R, Cortés-Gallegos V. Archives of andrology 28:3 pg 171-6.
[xxi] Drug-induced gynecomastia: an evidence-based review. Deepinder, F; Braunstein, GD (2012). Expert opinion on drug safety 11 (5): 779–795. doi:10.1517/14740338.2012.712109. PMID 22862307.
[xxii] Activation of the somatotropic axis by testosterone in adult males: evidence for the role of aromatization. Weissberger AJ, Ho KK. J Clin Endocrinol Metab. 1993 Jun;76(6):1407-12.





